Learn How Menopause Affects Your Bones & What You Can Do?
Menopause is when your menstrual cycle permanently stops. It often strikes women between the ages of 45 and 55. Do you know that menopause can affect your bone health as well? As people age, they lose bone mass or density, especially women who have gone through menopause. Minerals such as calcium are also lost from the bones. In the first five years following menopause, women might lose up to 10% of their bone mass on average. Hence, a woman's bone health is particularly crucial during this period.
Let us understand the effects of menopause on your bone strength and what precautions you should take to avoid bone issues at this stage of life.
Decoding the Connection between Menopause and Bone Health
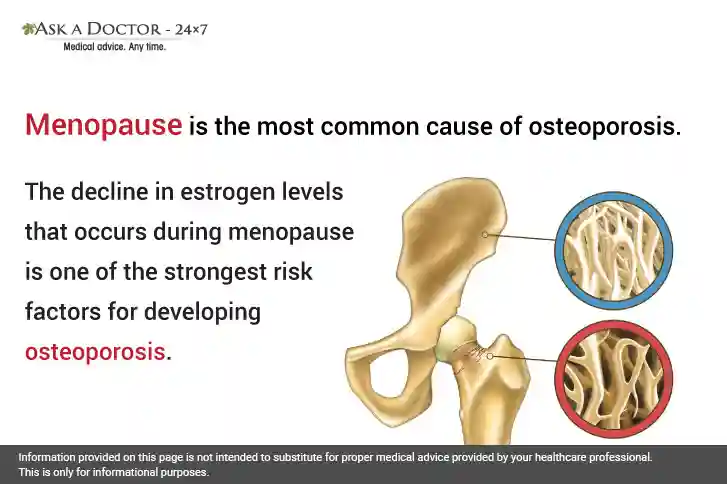
Menopause is the stage in a woman’s life that marks the end of her reproductive years. During this time, the female body goes through a variety of changes as a result of hormonal imbalances. Deterioration of bone health is one of the common side effects of menopause that causes brittle bones. This is due to a reduction in estrogen hormone, which is critical for maintaining both bone strength and bone density. Consequently, bone density begins to decline after menopause.
Also, when estrogen levels decline there is an imbalance between bone formation and breakdown, causing a decrease in bone density. A higher chance of breaking bones and decreased bone strength accompany this loss of bone density. Studies have shown that up to 20% of bone loss can occur during menopause.
What is Osteoporosis?
Osteoporosis means “porous bone.” In osteoporosis, the body is not only removing calcium from the bones but also not enough calcium is getting into the bones, causing the bones to become weak and brittle. It is often called a "silent disease," as initially, bone loss occurs with no apparent symptoms. People may only know that they have osteoporosis when their bones become so weak that a sudden strain, bump, or fall causes their bones to break or collapse a vertebra. According to statistics, 1 in 5 men and 1 in 3 women will have an osteoporotic fracture over the age of 50. Osteoporosis-related fractures most commonly occur in the hip, wrist, or spine.
Common signs and symptoms of osteoporosis are:
- Back pain
- Reduction in height over time.
- Fatigue, weakness, and a decreased capacity for activity due to muscle weakness.
- A bent-over position.
- Decreased mobility.
- Joint problems range from mild stiffness to arthritis (osteoarthritis).
- A bone that fractures far more frequently than anticipated.
How Osteoporosis is Diagnosed?
A bone density scan or DEXA scan is used to detect osteoporosis. It is a low-dose x-ray test that measures calcium and other minerals in your bones. It gauges bone density, or thickness, commonly in the region of the upper hip and lower spine.
A T-score from a DEXA scan indicates whether you have:
- Normal bone density
- A little amount of bone loss
- Significant loss of bone (osteoporosis)
It's critical to receive treatment for osteoporosis and undergo routine evaluations of your bone density.
How to Prevent Osteoporosis During Early Menopause
Lifestyle choices, including a healthy diet, regular exercise, and medication can assist in stopping more bone loss and lower your chance of fractures due to osteoporosis. The following should be kept in mind:
- Eat a balanced diet: A diet rich in calcium, protein, fresh fruits, and vegetables is crucial. As you age, women must take extra care to ensure they are getting adequate calcium and vitamin D. For strong, healthy bones, calcium is essential, and your body requires vitamin D to absorb calcium. Consult your healthcare practitioner about prescription medications if you have osteoporosis.
- Exercise: Regular weight-bearing, impact, and muscle-strengthening exercises maintain the strength of the bones. A moderate exercise routine can help you maintain strength, balance, and flexibility. Consult your physician before beginning a new fitness regimen.
- Take enough Vitamin D: Natural sunshine is pivotal to maintaining adequate vitamin D. You should also consider a vitamin D supplement in the winter months when you can’t get enough vitamin D from the sun.
- Go for menopausal hormone therapy (MHT): MHT can stop bone loss if you start taking it shortly after menopause, about the age of fifty.
- Avoid smoking: Smoking tobacco reduces bone mass and increases the risk of osteoporosis and fractures by creating an imbalance in bone turnover.
- Limit alcohol intake: Heavy alcohol intake decreases bone density, weakens bones, and causes changes in bone’s mechanical properties. Alcohol also interferes with the metabolism of vitamin D.
- Keep a weight check: Prevent obesity to keep your bones strong.
Conclusion
To conclude, menopause is a crucial time of transition for every woman that results in a variety of emotional and physical changes. The relationship between bone health and menopause must be clearly understood, as the effect on bone health at this stage is frequently disregarded. When going through menopause, modifying one's lifestyle can significantly enhance bone health. Also, consult your medical practitioner for further guidance or assistance, who can offer advice, suggest bone density testing, and discuss treatment.
Ask a Doctor to facilitate online consultation 24x7, you can send your questions related to osteoporosis and bone health to an Orthopedic Specialist online and get an answer within minutes.
Recently Answered Queries Related to Menopause & Women's Health Concerns
- Do Late Periods And Mood Swings Indicates Menopause?
- Am I at Greater Risk Of Ovarian Cancer If Had a Hysterectomy But Retained Ovaries?
- What Causes Shortness Of Breath And Chest Pain During Menopause?
- Suggest Treatment For Sharp Pain In The Abdomen
- Are Sweating Hot Flushes Menopause Symptoms?
- What Are The Side Effects Of Cortisone Injection?
- Are Vaginal Bleeding And Breast Pain Causes For Concern in a 59-Year-Old?
- Does Ovamit Cause Hot Flashes, Severe Headaches, And Bloating?
- Suggest Treatment For Dryness And Foul Odor In The Vagina
- Suggest Treatment For Recurring Vaginal Yeast Infections
Disclaimer: Information provided on this page is not intended to substitute for proper medical advice provided by your healthcare professional. This is only for informational purposes.
Ask a Specialist
Recent Questions


